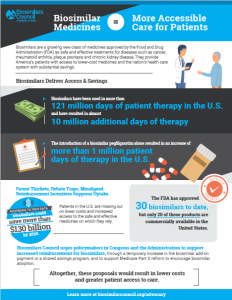
In recent years, significant attention has been given to the advent of biosimilars, a new class of medicines approved by the Food and Drug Administration (FDA) for the U.S. patient population. These medications deliver safe and effective care, with lower costs, for patients suffering from diseases such as cancer, rheumatoid arthritis, plaque psoriasis and chronic kidney disease.
Expanded Access Improves Potential to Increase Days of Therapy
Although the FDA has approved 30* biosimilars to date, only 20 of these products are available for patient use. These products have faced challenges resulting in suboptimal adoption due to brand biologic patent thickets that delay market entry, brand rebate traps and perverse reimbursement incentives that favor higher-priced brand medicines. As a result, patients in the U.S. are missing out on the benefits of biosimilars, including lower costs and increased access to the safe and effective medicines they rely on.
Yet, despite the slower than anticipated adoption, biosimilars have already saved patients and taxpayers $4.5 billion, highlighting the promise of savings from biosimilars.[1]
And as patient and provider experiences with these products increase, so does their understanding and acceptance of biosimilars. A new analysis completed by IQVIA on behalf of the Biosimilars Council found that biosimilars have been used in more than 121 million days of patient therapy. Further, the analysis concluded that biosimilars have resulted in almost 10 million additional days of therapy.
For example, the market launch of one biosimilar, pegfilgrastim, resulted in an increase of more than one million patient days of therapy. The increase in therapy days following the introduction of a biosimilar demonstrates that FDA-approved biosimilars promote patient access simply through their presence in the market because of their lower cost.
The availability of biosimilars has meant that many patients affected by cancer, chronic kidney disease and other chronic conditions have now been able to access treatment they otherwise would not have received. These results support the Biosimilars Council’s previous findings that biosimilars would result in additional access to care for more than one million patients.[2]
Biosimilar Adoption Results in Greater Savings
In addition to increasing patient access, biosimilars launch prices are on average 30% lower than that of the originator product, so patients will see lower out-of-pocket costs when a biosimilar is administered instead of the brand therapy. Collectively, the introduction and availability of biosimilars means that patient access is increased and patient costs are decreased–two goals shared by stakeholders across the health care spectrum.
However, more can be done to encourage biosimilar adoption. AAM and its Biosimilars Council urge policymakers in Congress and the Administration to support increased reimbursement for biosimilars, through a temporary increase in the biosimilar add-on payment or a shared savings program and to support Medicare Part D reform to encourage biosimilar adoption. Altogether, these proposals would build upon the additional 10 million days of therapy that biosimilars provide for U.S. patients, and result in lower costs and even greater access to care.
These policies, among others, can put the U.S. health care system on the right track toward widespread adoption and utilization of biosimilars, which offer equivalent clinical outcomes while promoting patient access and cost savings.